Risk Assessment Studies
Report No. 45
Dietary Iodine Intake in Hong Kong Adults
July 2011
Centre for Food Safety
Food and Environmental Hygiene Department
The Government of the Hong Kong Special Administrative Region
Correspondence:
Risk Assessment Section
Centre for Food Safety,
Food and Environmental Hygiene Department,
43/F, Queensway Government Offices,
66 Queensway, Hong Kong.
Email: enquiries@fehd.gov.hk
| Table of Contents |
|---|
| Executive Summary |
| Objectives |
| Background |
| Scope of Study |
| Methods |
| Results and Discussions |
| Conclusion and Recommendation |
| References |
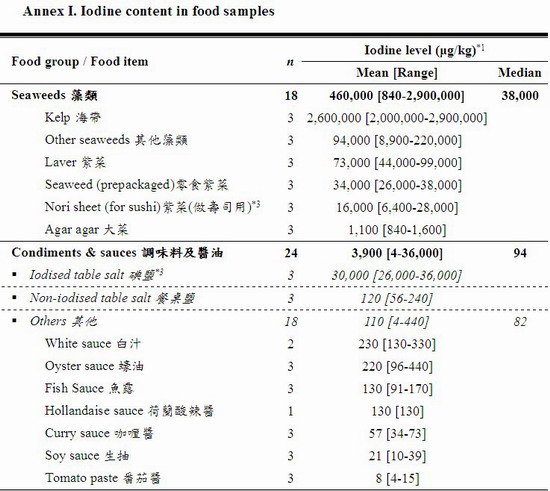
| Annex I: Iodine content in food samples |
| Annex II: Examples of food items being completely or partially mapped |
Risk Assessment Studies
Report No.45
Dietary Iodine Intake in Hong Kong Adults
EXECUTIVE SUMMARY
The Centre for Food Safety (CFS) has conducted a study on iodine content in local foods aiming to (i) examine the iodine levels in selected foods in Hong Kong, and (ii) estimate the dietary iodine intake in adults.
Iodine is an essential micronutrient required for normal thyroid function, growth and development. Its deficiency and excess both have adverse consequences on the body through effects on the thyroid gland. The thyroid gland requires trapping about 50-75 micrograms (μg) iodine daily to maintain an adequate supply of thyroid hormones. When daily iodine intake is below 50 μg threshold, goitre may develop. The Chinese Nutrition Society established the estimated average requirement (EAR) for iodine at 120 μg/day, the recommended nutrient intake (RNI) at 150 μg/day and the tolerable upper limit level (UL) at 1,000 μg/day for Chinese adults aged 18 years and above. These RNI and UL were the same as the World Health Organization (WHO)'s recommendations, but for pregnant/ lactating women WHO has revised the requirement of iodine in 2007 at 250 μg/day. Food is a major source of iodine intake, especially from seaweeds, seawater fish, and shellfish. The processing and cooking of food may cause iodine loss in foods.
The Study
Between February and April 2009, food samples were collected from the local retail food markets and restaurants to include foods commonly consumed. The levels of iodine were analysed in 271 samples from 11 groups, including (i) cereals & grains products, (ii) legumes and vegetables, (iii) meat and poultry, (iv) egg & egg products, (v) milk & milk products including frozen confections, (vi) fish, (vii) crustaceans and molluscs, (viii) non-alcoholic beverages, (ix) condiments & sauces (including non-iodised and iodised table salts), (x) sashimi & sushi, and (xi) seaweeds. Laboratory analysis for iodine was conducted by the Food Research Laboratory of the CFS. All food samples (edible portions) were analysed individually as purchased. In order to estimate the influence of cooking (e.g. stir-frying, steaming, boiling) on the iodine levels in foods, a total of 15 individual samples from five food items were analysed as raw and respective cooked foods.
Results
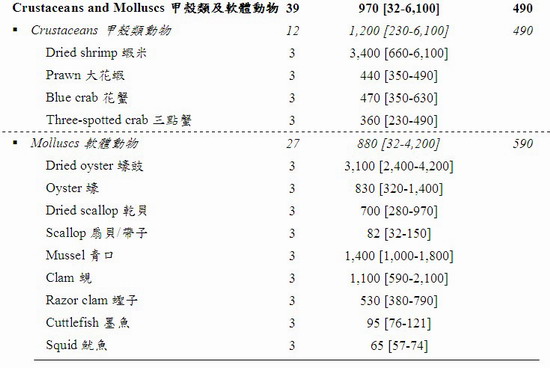
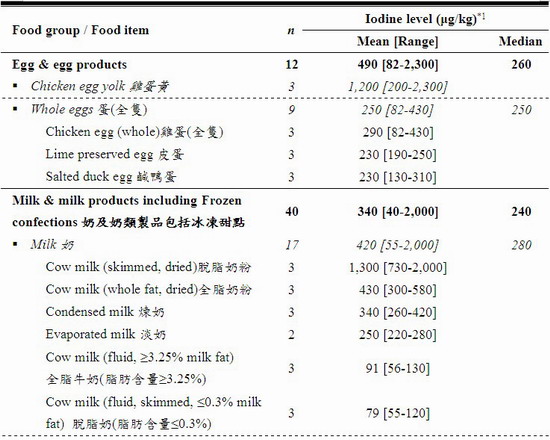
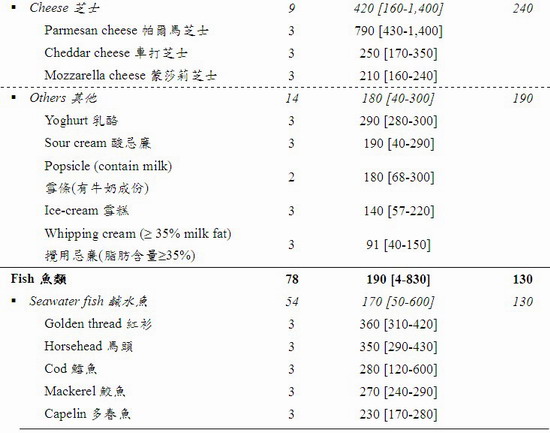
The iodine levels of the tested samples varied greatly from not detected (ND) to 2,900,000 μg per kilogram (kg) of food. Variation was also observed among different samples of the same food item. The food groups with the richest iodine content (mean [range]) were seaweeds (460,000 [840 – 2,900,000] μg/kg) and condiments & sauces (3,900 [4 – 36,000] μg/kg) particularly iodised salt (30,000 [26,000 – 36,000] μg/kg). After these were crustaceans and molluscs (970 [32 – 6,100] μg/kg), egg & egg products (490 [82 – 2,300] μg/kg), milk & milk products including frozen confections (340 [40 – 2,000] μg/kg), fish (190 [4 – 830] μg/kg), and sashimi and sushi (86 [28-140] μg/kg). A low level of iodine was found in meat and poultry (42 [ND – 480] μg/kg), cereals & grains products (13 [3 – 68] μg/kg), legumes and vegetables (8 [ND – 28] μg/kg), and non-alcoholic beverages (6 [ND – 13] μg/kg).
The median iodine dietary intakes from the 11 food groups in adults were estimated to be 44 μg/day and around 59% of the population had iodine intakes below 50 μg/day, the threshold for normal thyroid functioning. Only 5% adult population had iodine intake at the safe range (i.e. sufficient to prevent deficiency while avoiding toxicity), 93% had intake below RNI (the risk of inadequacy) and 2% had intake above UL (the risk of toxicity). It is understood if the local population took 5-10 g/day iodised salt (WHO recommends taking less than 5 grams of salt per day (about 1 teaspoon)), an extra 150-300 μg/day of iodine would be added to the diet, and the total dietary iodine intake would be above the RNI but below the UL.
Cooking had little or marked effects on the iodine levels in foods, depending on the cooking method. However, when taking the weight changes into account, the relative amount of iodine in the raw and cooked portions was mostly constant except for boiling foods as iodine may dissolve into water. The results were also consistent with other studies that more iodine is lost in boiling than in stir-frying or in steaming.
Conclusion and Recommendations
Iodine is present in many of the foods available locally but its content varied greatly within and among food groups. Seaweeds, iodised salt, seafoods, milk & milk products as well as egg & egg products were rich sources of iodine. The influence of cooking on the iodine level in foods was minimal, except for boiling as iodine dissolved into the soup. If iodised salt was taken as part of the diet, the dietary iodine intake in adults would be above the RNI but below the UL. Comprehensively assessing the iodine status of the local population using clinical and biochemical indicators as well as nutritional studies is urged.
Advice to consumers
- Eat a variety of high-iodine foods (e.g. seaweeds, seafoods, egg/egg products, milk/milk products) as part of a healthy balanced diet to ensure sufficient iodine intake.
- Follow WHO recommendation on taking less than 5 grams of salt per day, and replace non-iodised salt with iodised salt.
- To retain the maximum amount of iodine in foods, steam or stir-fry them with little oil, cook crustaceans intact, and add iodised salt just before serving the food.
- Apart from the above advice, women preparing for pregnancy and pregnant/lactating women shall seek advice from health professionals to assess the need of taking iodine supplements.
Advice to the trade
- Make iodised salt available for the public to choose and if possible provide clear instructions on its usage to minimise its iodine loss.
- When iodising salt, follow WHO recommendation of adding 20-40 mg iodine per kg of salt.
- Indicate on the label of salt if it is iodine-fortified and declare the amount of iodine on the label.
Risk Assessment Studies –
Dietary Iodine Intake in Hong Kong Adults
OBJECTIVES
This study aims to (i) examine the iodine levels in foods available in Hong Kong, and (ii) estimate the dietary iodine intake in adults.
BACKGROUND
2. Iodine is an essential micronutrient required for normal thyroid function, growth and development. When iodine intake falls below recommended levels, the thyroid may no longer be able to synthesize sufficient amounts of thyroid hormone. The resulting low level of thyroid hormones in the blood (hypothyroidism) is the principal factor responsible for damage to the developing brain and other harmful effects known collectively as iodine deficiency disorders (IDD). The World Health Organization (WHO) opines that the elimination of IDD is a critical development issue which should be given the highest priority by governments and international agencies, and recommends that countries conduct a national survey on the iodine status of the population every 3 to 5 years.[1,2]
3. Iodine deficiency and excess both have adverse consequences on the body through effects on the thyroid gland. The determination of the presence or absence of its deficiency or excess requires the integration of clinical, biochemical and nutritional data.[3] WHO recommended several clinical and biochemical indicators for assessing the iodine status of a population (e.g. thyroid size by palpation and/or by ultrasonography, urinary iodine (UI), blood thyroid stimulating hormone (TSH) and thyroglobulin levels).[1,4] However this study only confined to the nutritional aspect of estimating the iodine intake adequacy in the local adult population.
Dietary Sources of Iodine
4. Food, including water, is a major source of iodine intake. The iodine content of foods reflects background levels in the environment (e.g. soil, seawater). Naturally, foods such as seaweeds, seawater fish and shellfish are relatively rich in iodine. Milk/milk products as well as egg/egg products from countries adopting universal salt iodisation (USI) may be high in iodine. USI is the iodisation of salt for both human and livestock consumption as a way to eliminate IDD.[4] For vegetables, fruits and cereals, unless grown in soils naturally high in iodine or treated with iodine containing fertilisers, they are usually poor dietary sources of iodine.[5,6]
5. Food processing and cooking may cause varying levels of iodine loss in foods and iodised salt. The loss is estimated from 3% to 67%, depending on the cooking methods (e.g. boiling loses 37%, shallow frying loses 27%). For iodised salt, the loss is about 20%.[1,7-10]
Physiological Functions of Iodine
6. Iodine is essential for the synthesis of thyroid hormones (i.e. thyroxine T4 and triiodothyronine T3) by the thyroid gland. These hormones play a major role in the growth and development of the brain and central nervous system, and control several metabolic processes such as regulating energy production.[5]
7. Across the life-span, inadequate thyroid hormone production due to insufficient iodine intake is associated with a range of adverse health effects collectively termed as IDD, including damage to the developing brain, goitre (an enlarged thyroid), cretinism (severely stunted physical and mental development), hypothyroidism, and varying degrees of other growth and developmental abnormalities. Pregnant/ lactating women and infants/ young children are particularly vulnerable to IDD.[5] People living in areas affected by severe iodine deficiency may have an intelligence quotient (IQ) of up to 13.5 points below that of those from comparable communities in areas where there is no iodine deficiency. [1]
8. The average dietary requirement for iodine is determined by normal T4 production without stressing the thyroid iodide trapping mechanism or raising TSH levels. This requirement is suggested to be 91-96 micrograms iodide per day (μg/day) basing on iodine turnover and balance studies in euthyroid adults. The thyroid traps about 50-75 μg/day iodine to balance losses and maintain thyroid hormone synthesis in adults. When daily iodine intake is above the threshold of about 50 μg, the thyroid iodine content remains within normal limits, despite circulating plasma inorganic iodine may decrease. Below this threshold, the thyroid iodine content is depleted and goitre may develop.[11,12]
Safety Reference Values of Iodine Intake for Adults
9. WHO and many countries have set daily dietary iodine intake recommendations and tolerable upper intake levels (UL) for different population groups. For example, WHO recommended a requirement of iodine at 150 μg/day for adolescents/ adults and 250 μg/day for pregnant/ lactating women, and opined that for healthy adults, daily iodine intakes of up to 1,000 μg appear to be entirely safe. [1,5]
10. The Chinese Nutrition Society has set the estimated average requirement (EAR), the recommended nutrient intake (RNI), and the UL of iodine at 120, 150 and 1,000 μg/day respectively for Chinese adults aged 18 years and above. The Chinese RNI and UL levels are in line with those recommended by WHO.[1,13] The EAR is the average daily nutrient intake value that meets the needs of 50% of the healthy individuals in a particular age and gender group. The RNI is the daily intake, set at the EAR plus 2 standard deviations, which meets the nutrient requirements of almost all (97.5%) apparently healthy individuals in an age- and gender-specific population group. The UL of nutrient intake is defined as the maximum intake from food, water and supplements that is unlikely to pose risk of adverse health effects from excess in almost all apparently healthy individuals in an age- and gender-specific population group. The range of intakes between RNI and UL should be considered sufficient to prevent deficiency while avoiding toxicity.[14]
11. One way of assessing dietary iodine intake deficient or excess in a population is by comparing the dietary iodine intake of a population with the EAR and UL of that particular population.[14] The US Institute of Medicine suggested an EAR cut-point method by simply counting how many individuals in the group of interest have usual intakes below the EAR. That proportion is the estimate of the proportion of individuals in the group with inadequate intakes. Similarly, by determining the proportion of the group with intakes above the UL, the proportion potentially at risk of adverse health effects from excess nutrient intake can be estimated.[15]
12. In this study, the dietary iodine intake result was compared with the EAR, RNI, and UL set by the Chinese Nutrition Society.[13] This is assuming that the local population has similar iodine requirements as the mainlanders, since the majority of Hong Kong people are Chinese.
International and Local Situations on Iodine Status
13. Iodine deficiency is an international health concern. It is estimated that about 70% of households throughout the world have access to (and use) iodised salt and more than 170 countries have committed to USI.[1,16] WHO considers iodine deficiency a worldwide public health problem basing on relevant biochemical and clinical data. Extrapolating the data from the schoolage children (6-12 years) to the general population, about 31% of the world's population have insufficient iodine intakes with South-East Asia and Europe being the most affected regions.[1,4] Various mandatory and voluntary population measures (e.g. USI, fortified foods or salt with iodine) have been adopted by different place to eliminate iodine deficiency.
14. Whilst some places have successfully kept IDD at bay (e.g. the US, the UK, the Netherlands, Switzerland), others have stepped-up efforts to prevent IDD re-emergence (e.g. Australia, New Zealand).[4,17-19] In the US excessive or inadequate iodine intake is not a public health concern based on epidemiological (e.g. total diet studies (TDS), core food studies) or clinical evidence and that monitoring the diet for iodine intake is not very useful.[15,17,20] Based on evidence (e.g. TDS, retail surveys, National Diet and Nutrition Survey), iodine intake is unlikely to pose a risk to health as a result of excessive intake in the UK.[18,21-23] Contrarily, using UI in parallel with iodine intake data from TDS is useful to track the iodine status in the population (includes pregnant/lactating women and infants/children). Australia and New Zealand found iodine inadequacy since the 80's and implemented mandatory iodine-fortification in bread using iodised salt in September 2009.[6,19,24,25]
15. In Mainland China IDD remains an important public health concern even though iodised salt has been introduced since 1995 which has greatly reduced its overall prevalence. However, in areas where the iodised salt coverage rate is poor including some coastal provinces, pregnant women are at a higher risk of IDD. Where the drinking water iodine level is below 150 μg/L, without the consumption of iodised salt, over 97% of the residents would have iodine intake below the EAR for Chinese adults. In these areas iodised salt contributed to about 80% of dietary iodine intake. Whereas in areas where iodine level in drinking water was above 150 μg/L, without the consumption of iodised salt, over 98% of the residents would have iodine intake above the RNI for Chinese adults; water contributed to about 90% of dietary iodine intake.[26,27]
16. Locally, there is limited information on the dietary iodine intake data. The Expert Panel Group on Iodine Deficiency Disorders in Hong Kong (the Panel) published a consensus statement in 2003.[28] The Panel opined that borderline iodine deficiency existed in the expectant mothers and urged for a comprehensive survey on iodine content of food items in Hong Kong. The paper has reviewed available data on the study of IDD of the local population subgroups. First, studies using UI and cord blood TSH levels as indicators reported that pregnant women and neonates may have mild iodine deficiency and high incidence of transient neonatal hypothyroidism. Second, studies using UI and goitre incidence as indicators reported that adolescents and children were iodine adequate. Lastly, studies using UI as an indicator reported that adults and elderly were borderline iodine sufficient. Local data on iodine status is scarce. Data on clinical cases of IDD is lacking and local hospitals do not collect UI data systematically.
Information about Iodine Content in Foods
17. Before this study, there were only two reports about the iodine content in local foods. In 1998, the Consumer Council (CC) reported the iodine content in 146 foods (e.g. seafood, salt, seaweed products, milk). CC commented that some seaweed snacks contained very high levels of iodine and children below 12 years consuming 2g (about 7-8 small slices) of them would have exceeded the WHO recommended daily iodine intake for this age-group (i.e. 120 μg/day).[29] In 2005, the Food and Environmental Hygiene Department (FEHD) reported the level of iodine in 74 table/cooking salt samples analysed in a joint study with CC. Almost all salt products (70 samples) that were not labelled as iodised had iodine content below the limit of detection (LOD) at 500 μg/kg, and the 3 products labelled as iodised salt had iodine ranged 31,000 – 43,000 μg/kg.[30] Together with the present study, these results could be useful for monitoring the iodine content in local foods.
SCOPE OF STUDY
18. This study covered 11 food groups, namely (i) cereals & grains products, (ii) legumes and vegetables, (iii) meat and poultry, (iv) egg & egg products, (v) milk & milk products including frozen confections, (vi) fish, (vii) crustaceans and molluscs, (viii) non-alcoholic beverages, (ix) condiments & sauces (including non-iodised and iodised table salts), (x) sashimi & sushi, and (xi) seaweeds.
METHODS
Sampling
19. Between February and April 2009, food samples were collected from the local retail food markets and restaurants in Hong Kong Island, Kowloon, and the New Territories to include foods commonly consumed. Foods were selected with reference to the results of the Hong Kong Population-based Food Consumption Survey 2005-2007 for the population aged 20-84 years (FCS).[31] A total of 271 samples from 11 food groups (i.e. 92 food items, each with 3 samples unless otherwise stated) were collected. The list of food items covered in each group is shown in Annex I.
Laboratory Analysis
20. Laboratory analysis was conducted by the Food Research Laboratory (FRL) which is experienced in analysing nutrients in foods. Only the edible portions of all food samples were analysed individually for iodine content using an in-house method validated by FRL. Food sample was homogenised and weighed. After enzymatic digestion, the sample was extracted by tetramethylammonium hydroxide (TMAH). The extract was subsequently analysed by Inductively Coupled Plasma Mass Spectrometer. Pre-packaged and ready-to-eat items were analysed directly as purchased. The edible portion of raw food samples was rinsed with distilled water if necessary.
Effects of Cooking on Iodine Levels in Selected Foods
21. The influence of cooking on the iodine level in foods was estimated using a total of 15 individual samples from five food items, namely Golden thread (fish), prawn, kelp, egg, and tap water. Fish, prawn and kelp were cut laterally into halves, cleaned and weighed before analysed. The cooking methods used were stir-frying without oil (fish and egg), steaming (egg), and boiling (prawn, kelp, and tap water).
Data Analysis
Data Interpretation
22. For iodine content in foods, the data was reported as μg/kg of edible portion, rounded to 2 significant figures. Values below LOD (2 μg/kg) were reported as Not Detected (ND). When calculating an arithmetic mean concentration of iodine in the same type of food, the ND results were allocated to 1 μg/kg (i.e. half of LOD).
23. For the effects of cooking on iodine levels in selected foods, the concentration of cooked food samples was corrected by the weight change in cooking and reported as percentage of change (%).
Dietary Iodine Intake Estimation
24. To estimate the dietary iodine intake of the population, two pieces of information were used: (i), the amount of each food item consumed by each FCS respondent (i.e. the mean of the 2 non-consecutive 24-hour dietary recalls (24-hr recall) in g/day), and (ii) the mean iodine levels among the sample of the same food items analysed in the 11 food groups. According to FCS, the average consumption amount of all foods by Hong Kong adults was 2,980 g/day (about 38% was from solid foods), of which 88.2% (i.e. 2,628 g/day) was mapped for iodine levels and included in the dietary iodine intake estimation.
25. Each FCS respondent's daily iodine intake was calculated by summation of iodine intake from individual food items being consumed, the amount of which was estimated by multiplying the respondent's consumption amount of a food item with the assigned mean iodine level of that food item. Since the distribution of iodine intake in the population was skewed, the median dietary intake of iodine in adults was reported.
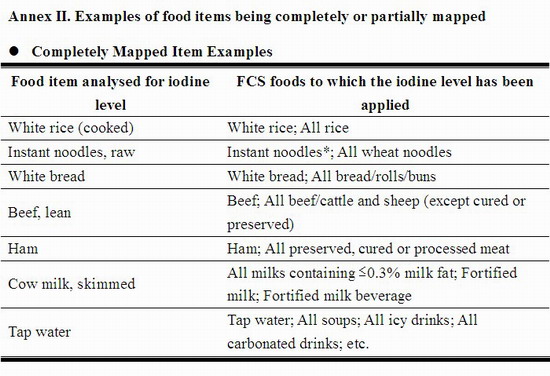
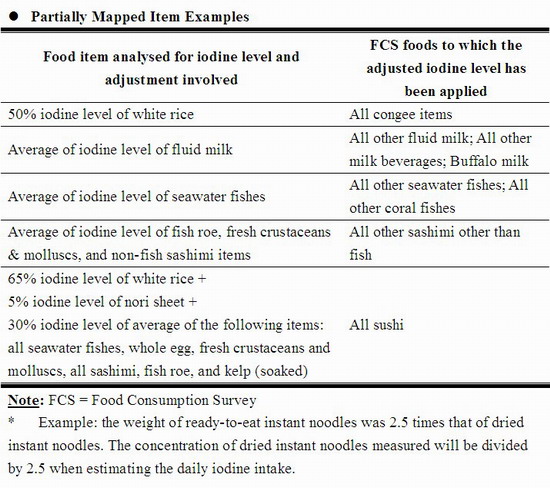
26. There were approximately 1,400 food items reported being consumed in the FCS but only 92 food items were analysed in this study; thus, a "mapping" procedure was adopted using two main principles: (i) for completely mapped items (i.e. those items being consumed or items similar to them have been analysed for iodine content), the mean iodine content of the three individual food samples analysed was used as their iodine content; and (ii) for partially mapped items, their iodine contents were estimated by comparing with relevant food items being analysed and calculating the respective contents by proportion. Examples of these items are outlined in Annex II. As the FCS data represented the amount of food as consumed, wherever relevant, yield factors were applied to adjust for the weight of the dried or raw foods from as purchased state (e.g. dried instant noodles) into as consumed state.[8]
RESULTS AND DISCUSSIONS
Iodine Content in Foods
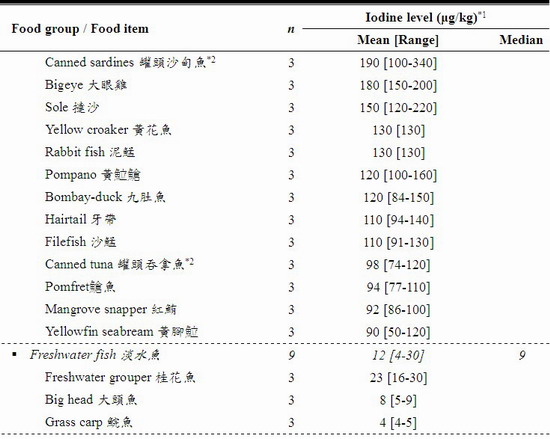
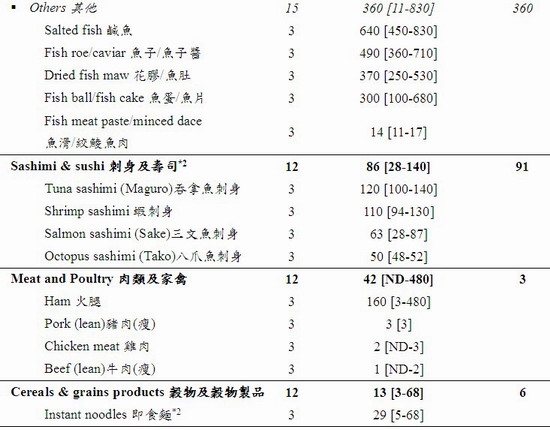
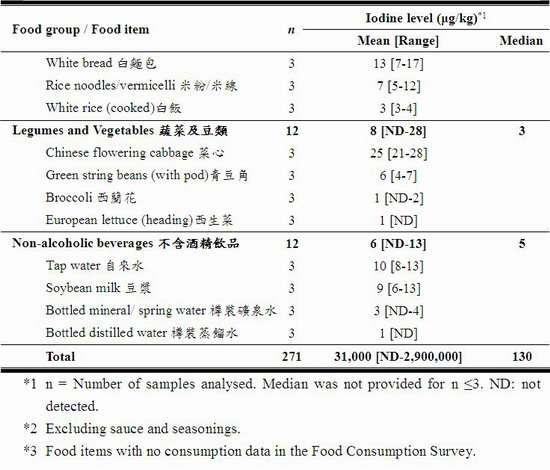
27. A total of 271 samples were tested for iodine. The results are summarised in Table 1 and the details in Annex I. The iodine level in the analysed foods varied among food groups as well as within the same food group.
28. The results showed a wide range of iodine levels in these foods (from ND to 2,900,000 μg/kg). The food groups with the richest iodine content (mean [range]) were seaweeds (460,000 [840 – 2,900,000] μg/kg) and condiments & sauces (3,900 [4 – 36,000] μg/kg) particularly iodised salt (30,000 [26,000 – 36,000] μg/kg). After these were crustaceans and molluscs (970 [32 – 6,100] μg/kg), egg & egg products (490 [82 – 2,300] μg/kg), milk & milk products including frozen confections (340 [40 – 2,000] μg/kg), fish (190 [4 – 830] μg/kg), and sashimi and sushi (86 [28-140] μg/kg).
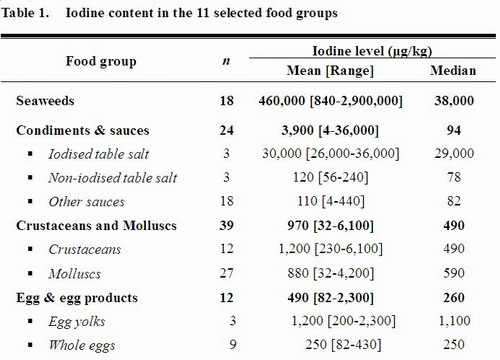
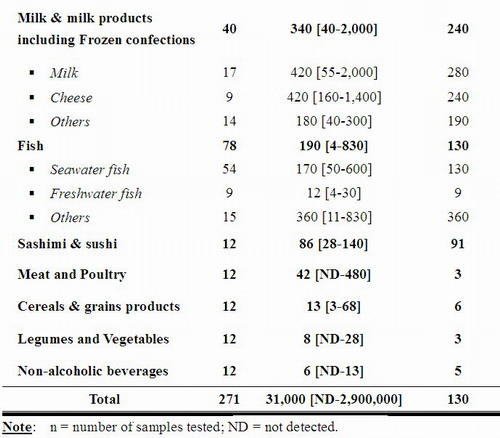
29. Most seaweed and seaweed products contained very high iodine levels. For example, the mean iodine content of prepackaged seaweed snacks was 34,000 μg/kg. Consuming one medium individual pack of 2.5-3.0 g would have contributed to about 57%-68% of WHO recommended daily iodine intake for healthy adults; a bigger pack would have easily met WHO's daily recommendation; and consuming about 10 packs would have exceeded the Chinese UL of 1000 μg/day. Furthermore, the mean iodine level of dried kelp was 2,600,000 μg/kg; consuming 1 g of dried kelp would almost reach a level tripled the Chinese UL. For healthy adults, occasional high intake of these products may not pose risk to the body, however, members of the general population are advised not to routinely exceed the UL for a long time.[15] Soaking the dried kelp and discard the water will lower the iodine level.
30. The iodine content in the table salt (range 56-240 μg/kg) and iodised salt (range 26,000-36,000 μg/kg) shows vast difference as reported previously in the CC and FEHD studies.[29,30] The locally available iodised salt samples were well within the range of 20,000-40,000 μg of iodine per kg of salt as recommended by WHO.[32] Among the three iodised salt samples purchased, only one has voluntarily declared the iodine level and provided instructions of using the product to minimise iodine loss (e.g. add iodised salt just before serving the food) on the food label.
31. The iodine content in seawater fish was higher than that in freshwater fish, and the iodine content in egg yolk was higher than that in whole egg. These findings were generally in line with the literature, which found that seawater fish had about 6-fold higher iodine level than freshwater fish; and in egg about 87-96% of iodine was in the yolk.[33,34]
32. A low level of iodine was found in meat and poultry (42 [ND – 480] μg/kg), cereals & grains products (13 [3 – 68] μg/kg), legumes and vegetables (8 [ND – 28] μg/kg), and non-alcoholic beverages (6 [ND – 13] μg/kg). The average iodine content of drinking water was 10 μg/L.
Daily Iodine Intake in the Population
Risk on Insufficient Iodine Intake
33. As evident in the mean and percentile distributions in Table 2, the dietary iodine intake distribution in the population was skewed (mean 127 μg/day, median 44 μg/day), thus the median value was reported. No adjustment of the intake figures was made although only 88.2% of foods were covered in the mapping because the remaining 11.8% of food intake (about 352 g/day) were foods which were likely to contain insignificant amounts of iodine (e.g. fruits, oils and spreads) as reported in the literature or some food composition databases.[35]
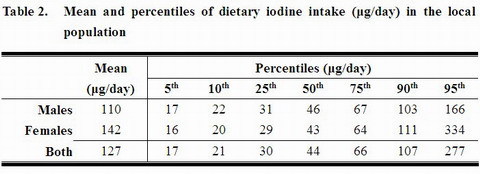
34. Around 59% of the population had iodine intakes below 50 μg/day, the threshold for normal thyroid functioning.[11] Further breakdowns of the distribution of dietary iodine intake in the 12 age-gender subgroups are shown in Table 3. Overall, no particular trend was shown in the median iodine intake among the different age and gender groups.
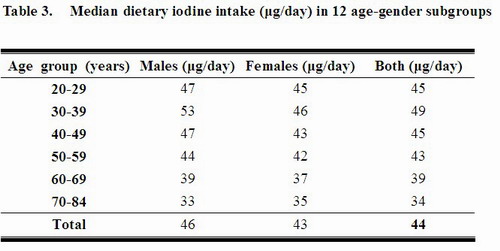
35. The proportion of the population with iodine intake below RNI, between RNI and UL, and above UL was 93%, 5%, and 2%, respectively. By using the EAR cut-point method, about 91% of the population had iodine intakes below EAR. A very low proportion of the population (about 5%) had iodine intakes sufficient to prevent deficiency while avoiding toxicity, i.e. between RNI and UL. The pattern was similar in both genders and in the 12 age subgroups.
36. In Mainland China, the dietary iodine intake level is affected by the geographical location, the drinking water iodine level, and the use of iodised salt etc.. The 2009 Iodine Intake in Coastal Areas Study reveals that in Shanghai, the mean iodine intake of a reference man* was 226 μg/day. If the contribution of iodised salt was excluded (estimated to be about 64%), the mean dietary iodine intake would only be 81 μg/day which would be far below the RNI. Furthermore, agglomerated data show that where the drinking water iodine level was below 150 μg/L, if iodised salt was not consumed, over 97% of the residents would have iodine intake below EAR; in these areas iodised salt contributed to about 80% of dietary iodine intake.[26] This implies the importance of USI in coastal areas and in low water iodine level areas such as in Hong Kong.
*A reference man is defined as an adult male, 19-59 years of age, 65 kg of body weight and undertaking very light physical work.
37. The above crude estimation on dietary intake suggested that assuming only the 11 food groups and non-iodised salt were consumed, most subgroups in the population might have inadequate iodine intakes, which echoes with the intake of people living in low water iodine level areas and excluding iodised salt in the diet in Mainland China. The iodine level in the local diet may not be sufficient to provide iodine for some surveyed respondents unless iodine rich foods and iodised salt are included in the diet. The population as a whole may need to increase the types and amounts of foods rich in iodine (e.g. seaweeds, seafoods including seawater fish, milk/milk products).
Risk on Excessive Iodine Intake
38. The UL was used to estimate roughly the percentage of adults at potential risk of adverse effects of overconsuming iodine. The high iodine intake (95th percentile) adults consumed 277 μg/day, which was about 30% of the UL (Table 2). This estimation had not covered iodine from sources other than the 11 food groups, such as supplements. About 2% of the population had iodine intakes above UL, which was expected with the skewed iodine intake data and possibly high intake of seaweed or seaweed-containing foods during the FCS survey period. Nonetheless, potential toxicity from excessive iodine intakes seems not a concern from the current assessment. An UL is not a threshold of toxicity but may be exceeded for short periods without an appreciable risk to the health of the individuals concerned.
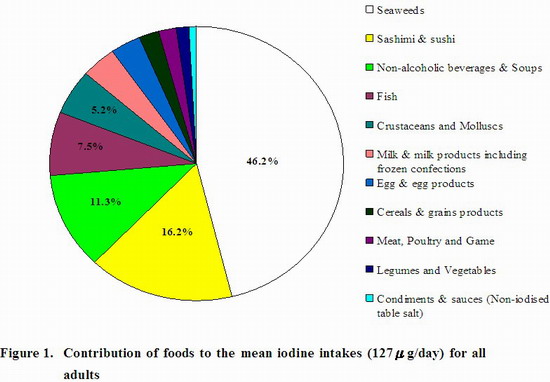
Contribution of Iodine Intake in Foods
39. The estimated contribution of iodine intake from different food groups (mean 127 μg/day) are shown in Figure 1 for all adults. Seaweed was the major source (46.2%) of iodine intake, even though it was consumed in a very small amount on average by the population (about 0.2 g/day) and only about 4.0% and 0.1% of the population reported consuming seaweed and seaweed snacks. Sashimi and sushi was the second major contributor of iodine (16.2%), possibly because of the seaweeds and seafoods ingredients. Other food groups that made important contribution to dietary iodine intake were the non-alcoholic beverages and soup group (11.3%) owing to its consumption in relatively large quantities, the fish group (7.5%) especially from the seawater fish, as well as the crustaceans and molluscs group (5.2%).
40. There were concerns that using the 24-hr recall might have over- or under-estimated the intake of iodine. Information from the 110-item food frequency questionnaire (FFQ) conducted in the FCS was used to provide another perspective of food consumption on food items that have been specifically asked for. The FFQ attempts to understand intake over the long term but in a cruder fashion than that of the shorter term 24-hr recall.
41. Seaweed intake (including laver and kelp), the major source of iodine intake, was captured in FFQ. Using the FFQ data to estimate the dietary iodine intake from seaweed per se instead of the 24-hr recall data, the rough estimation shows that the proportion of the population with daily iodine intake below the 50 μg (goitre may develop) will be decreased from 59% to about 25% and that below the 150 μg RNI will be decreased from 93% to about 67%. Nevertheless, readers should be cautioned in combining the food consumption estimates from 24-hr recall and from FFQ, and their respective limitations.
42. Regardless of the methods used, both 24-hr recall and FFQ data showed that the majority of the population has insufficient iodine intake from the diet, although the magnitude of deficiency is smaller when estimated from FFQ data.
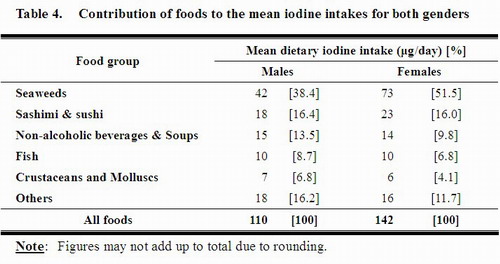
43. As shown in Table 4, the top four iodine contributors of both genders remained the same as that in the whole population, i.e. seaweeds, sashimi and sushi, non-alcoholic beverages and soup, and fish.
Contribution of Iodised Salt to the Total Iodine Intake in the Local Diet
44. In the FCS, the pattern of iodised salt consumption was not assessed and the mean salt intake of the population seemed underreported (1.7 g/day). Other studies have reported much higher salt intakes (e.g. Mainland China 12 g/day, the UK 8.6 g/day) than the present study.[36,37] In view that the contribution of non-iodised salt to dietary iodine intake was insignificant (about 0.2 μg/day) because of its low iodine content (120 μg/kg), the total dietary iodine intake level in the population was re-assessed by assuming iodised salt was consumed. It is understood if the local population consumed 5-10 g/day iodised salt, a level estimated by the WHO on worldwide average salt intake amount,[32] and using the iodised salt mean iodine level (30,000 μg/kg) measured in this study, an extra 150-300 μg/day of iodine would be added to the diet. The total dietary iodine intake of the population would then be above the RNI but below the UL.
Pregnant/Lactating Women and Iodine Intake
45. In spite of the possible risk of inadequate dietary iodine intakes in adults found in this study, whether the iodine status in Hong Kong is borderline deficient as suggested by the Panel for expectant mothers would require biochemical testings (e.g. UI) and clinical examinations (e.g. goitre, cretinism) in the population to diagnose IDD.[4,28,38]
46. Pregnant and lactating women who are more prone to suffer from iodine deficiency could eat iodine rich foods. If indicated, women preparing for pregnancy and pregnant/ lactating women could also choose iodised salt as an alternative dietary source of iodine. Iodine supplements should also be considered. However, they should seek advice on their individual dietary needs from health professionals beforehand.
Effects of Cooking on Iodine Levels in Selected Foods
47. A total of 15 samples (edible portion) were tested for iodine after being cooked by different methods (stir-frying, steaming and boiling), and the results are summarised in Table 5. When taking the weight changes into account, the relative amount of iodine in the raw and cooked parts kept nearly constant except for boiled foods. Iodine was almost all retained after stir-frying or steaming which was similar to that reported in other studies.[7,9,10]
48. Depending on the type of foods, this study found that boiling decreased the amount of iodine by 6% to 91%. As 83% of the iodine in the kelp dissolved into the soup, if all the soup was also included in the analysis, over 90% of iodine remained in the kelp and soup. The result was consistent with literature data that iodine loses more in boiling than in frying or in steaming. To minimise the loss of iodine in the foods, choose steaming or stir-frying without oil. If boiling is deemed necessary, cook the food (e.g. prawns with their shells) intact.[7,9,10]

Limitations of the Study and Suggestions for Further Studies
49. This study only analysed the iodine levels in a limited number of food items, in which three samples of each were taken, from 11 food groups. Not all foods and food groups (e.g. fruits) commonly eaten and containing iodine have been tested. So, increasing the number of samples for each food and food types for laboratory analysis could provide a more precise estimate of the level of iodine in foods.
50. Furthermore, some food items with high iodine content but only occasionally consumed by the population might not be recorded in the 24-hr recall on the two interview days. It might lead to underestimation of iodine intake. FFQ could provide supplementary information on the consumption pattern of these foods (e.g. seaweed); however, the results could only provide rough estimations of the dietary iodine intake from the particular food items.
51. Both 24-hr recall and FFQ have strengths and weaknesses. Although both methods do not affect the respondents' customary eating patterns, they depend on memory for accurate intake report. Using FFQ has the advantage of estimating selected foods usually eaten over a longer period, e.g. 12 months; however, it provides limited possibilities for food specification, and quantification of food intake may be inaccurate because of poor estimation of recall portions or use of standard portion size. On the other hand, using the open-ended 24-hr recall has the advantage of collecting the consumption amount of all food items in more detailed; nevertheless, the usual intake of an individual cannot be assessed from 1 day recall due to day-to-day variation, as it only reflects the consumption of food items over a short period, e.g. average of 2 days. Moreover, the portion size is difficult for the respondents to estimate accurately.[39] To comprehensively assess the iodine content in food and iodine intake of the population, more studies are required.
52. The pattern of iodised salt consumption was unknown and the mean salt intake of the population seemed underreported, therefore, the dietary intake of iodine may be underestimated. Strategies to ensure the accuracy of data captured from FCS on salt intake and the salt type is warranted for iodine intake assessment.
53. Estimation of iodine intake in populations at risk of IDD, such as pregnant women and young children, was not possible due to a lack of comprehensive local food consumption data in these groups. More studies on these groups are urged and biochemical testings (e.g. UI) and clinical examinations (e.g. goitre, cretinism) shall be incorporated to provide a comprehensive view of the iodine status.
54. The prevalence of IDD in the local population needs to be established, from studies using biomarkers for assessing iodine status and to include more groups besides the vulnerable ones (i.e. infants/ young children and pregnant/ lactating women). Besides conducting ongoing TDS (including iodine as one of the nutrients) to monitor and verify the dietary iodine intake situation in the population, the findings need to be confirmed by continual investigations of iodine status and clinical diagnosis (e.g. UI excretion, thyroid gland size, blood TSH and T4 levels) as practicised internationally (e.g. Mainland China, Australia and New Zealand).[6,25,26]
CONCLUSION AND RECOMMENDATIONS
55. Iodine is present in many of the foods available locally and its content varied greatly within and among food groups. Seaweeds, iodised salt, seafoods, milk & milk products as well as egg & egg products were rich sources of iodine. The influence of cooking on the iodine levels in foods was minimal, except for boiling as iodine dissolved into the soup. About 93% population has iodine intake less than Chinese RNI. If iodised salt was taken as part of the diet, the dietary iodine intake in adults would be above the RNI but below the UL. Comprehensively assessing the iodine status of the local population using clinical and biochemical indicators as well as nutritional studies is urged.
Advice to consumers
56. The public is advised:
- To eat a variety of high-iodine foods (e.g. seaweeds, seafoods, egg/egg products, milk/milk products) as part of a healthy balanced diet to ensure sufficient iodine intake.
- To follow WHO recommendation on taking less than 5 grams of salt per day (about 1 teaspoon), and replace non-iodised salt with iodised salt
- To retain the maximum amount of iodine in foods by steaming or stir-frying them with little oil, cooking crustaceans intact, and adding iodised salt just before serving the food.
- Apart from the above advice, women preparing for pregnancy and pregnant/lactating women shall seek advice from health professionals to assess the need of taking iodine supplements.
Advice to the trade
57. Members of the trade are advised:
- To make iodised salt available for the public to choose and if possible provide clear instructions on its usage to minimise its iodine loss (e.g. add iodised salt just before serving the food).
- When iodising salt, follow WHO recommendation of adding 20-40 mg iodine per kg of salt.
- Indicate on the label of salt if it is iodine-fortified and declare the amount of iodine on the label.
REFERENCES
[1] World Health Organization (2007) Assessment of iodine deficiency disorders and monitoring their elimination: A guide for programme managers (3rd Ed.). Available at URL http://whqlibdoc.who.int/publications/2007/9789241595827_eng.pdf.
[2] World Health Organization (2010) 63rd World Health Assembly Progress reports (A63/27): Sustaining the elimination of iodine deficiency disorders (resolution WHA60.21). Available at URL http://www.who.int/nutrition/topics/A63.27_idd_en.pdf
[3]Jackson, M.J. (1999) Diagnosis and detection of deficiencies of micronutrients: Minerals. British Medical Bulletin 55: 634-642.
[4] World Health Organization. (2004) Iodine status worldwide. WHO Global Database on Iodine Deficiency. Available at URL http://whqlibdoc.who.int/publications/2004/9241592001.pdf.
[5] World Health Organization. (2004): Chapter 16: Iodine. In Vitamin and Mineral Requirements in Human Nutrition (2nd Ed.). Available at URL http://whqlibdoc.who.int/publications/2004/9241546123_chap16.pdf.
[6] Food Standards Australia New Zealand. (2008) The 22nd Australian Total Diet Study. Available at URL http://www.foodstandards.gov.au/_srcfiles/ATDS.pdf.
[7] Goindi, G., Karmarkar, M.G., Kapil, U., Jagannathan, J. (1995) Estimation of losses of iodine during different cooking procedures. Asia Pacific Journal of Clinical Nutrition 4: 225-227.
[8] 楊月欣主編。 (2006) 《食物營養成分速查》。 出版社: 人民日報。[in Chinese only].
[9] Deraniyagala, S., Perera, W. (1999) Iodine in marine prawns and its fate on boiling. Journal of the National Science Foundation of Sri Lanka 27: 197-202.
[10] Karl, H., Basak, S., Ziebell, S., Quast, P. (2005) Changes of the iodine content in fish during household preparation and smoking. Deutsche Lebensmittel-Rundschau 101: 1-6.
[11] Zimmermann, M.B. (2009) Iodine deficiency. Endocrine Reviews 30: 376-408.
[12] 葛可佑總主編。 (2001) 《中國營養科學全書(上冊)》(An Overview of Nutrition Sciences): 第八章 微量元素; 第三節 碘。出版社:中國人民衛生出版社。[in Chinese only].
[13] 中國營養學會編著。 (2001) 《中國居民膳食營養素參考攝入量Chinese DRIs》(簡要本)。出版社:中國輕工業。[in Chinese only].
[14] World Health Organization. (2004): Chapter 1: Concepts, definitions and approaches used to define nutritional needs and recommendations. In Vitamin and Mineral Requirements in Human Nutrition (2nd Ed.). Available at URL http://whqlibdoc.who.int/publications/2004/9241546123_chap1.pdf.
[15] Institute of Medicine (2001) Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Available at URL http://www.nap.edu/catalog.php?record_id=10026.
[16] The International Council for Control of Iodine Deficiency Disorders (ICCIDD), The Micronutrient Initiative (MI), Opportunities for Micronutrient Interventions (OMNI), The Program Against Micronutrient Malnutrition (PAMM), The United Nations Children's Fund (UNICEF), The United States Agency for International Development (USAID), (WHO)., T.W.H.O. (1999) Assessing Country Progress in Universal Salt Iodisation Programs -- Iodized Salt Program Assessment Tool (ISPAT). Available at URL http://www.micronutrient.org/resources/Salt_CD/4.0_useful/4.1_fulltext/pdfs/4.1.3.pdf.
[17] US Department of Agriculture (1995) Third Report on Nutrition Monitoring in the United States: Volume 2. Available at URL http://www.ars.usda.gov/SP2UserFiles/Place/12355000/pdf/nutri95_2acc.pdf.
[18] UK Food Standards Agency (2010) National Diet Nutrition Survey: Headline Results from Year 1 (2008/2009). Available at URL http://www.food.gov.uk/science/dietarysurveys/ndnsdocuments/ndns0809year1.
[19] Food Standards Australia New Zealand (2010) Fact sheets 2010 - Iodine in food. Available at URL http://www.foodstandards.gov.au/scienceandeducation/factsheets/factsheets2010/
iodineinfoodoctober24961.cfm.
[20] US Department of Agriculture (1995) Third Report on Nutrition Monitoring in the United States: Executive Summary. Available at URL http://www.ars.usda.gov/SP2UserFiles/Place/12355000/pdf/tronm.pdf.
[21] UK Food Standards Agency (2008) Retail survey of iodine in UK produced dairy foods. Available at URL http://www.food.gov.uk/science/surveillance/fsisbranch2008/fsis0208.
[22] UK Food Standards Agency (2003) National Diet and Nutrition Survey: Adults aged 19 to 64, Volume 3 2003. Available at URL http://www.food.gov.uk/multimedia/pdfs/ndnsv3.pdf.
[23] UK Food Standards Agency (2000) 1997 Total Diet Study - Fluorine, Bromine and Iodine (Number 05/00). Available at URL http://www.food.gov.uk/science/surveillance/fsis2000/5tds.
[24]New Zealand Ministry of Health (2000) 1997/98 New Zealand Total Diet Survey. Part 2: Elements. Selected Contaminants & Nutrients. Available at URL http://www.moh.govt.nz/moh.nsf/0/A48868055568B2814C2568B100823CEF/
$File/ElementsFinal.pdf.
[25] New Zealand Food Safety Authority (2005) 2003/04 New Zealand Total Diet Survey Full Report. Available at URL http://www.foodsafety.govt.nz/elibrary/industry/2003-04-nztds-full%20report.pdf.
[26] 中華人民共和國衛生部。 (2010) 《中國食鹽加碘和居民碘營養狀況的風險評估》(Salt iodization and risk assessment of iodine status in Chinese population) 。[in Chinese only]. Available at URL http://www.moh.gov.cn/publicfiles///business/cmsresources/mohwsjdj/
cmsrsdocument/doc9250.pdf.
[27] 中華人民共和國衛生部。 (2010) 《衛生部專家否認居民攝入碘過量》。[in Chinese only]. Available at URL http://www.moh.gov.cn/sofpro/cms/previewjspfile/wsb/
cms_0000000000000000207_tpl.jsp?requestCode=48256&CategoryID=527.
[28] Expert Panel Group on Iodine Deficiency Disorders in Hong Kong (2003) Consensus statement on iodine deficiency disorders in Hong Kong. Hong Kong Medical Journal 9: 446-453.
[29] Consumer Council (1998) Test on 146 foods and snacks to advise consumers on adequacy of iodine intake. CHOICE: # 264 (215 October 1998).
[30] Food and Environmental Hygiene Department & Consumer Council (2005) Study on salt in local market. Abstract available at URL http://www.cfs.gov.hk/english/programme/programme_rafs/
programme_rafs_fci_01_01.html.
[31] Food and Environmental Hygiene Department (2010) Hong Kong Population-based Food Consumption Survey 2005-2007. Final Report. Available at URL http://www.cfs.gov.hk/english/programme/programme_firm/files/
FCS_final_report.pdf.
[32] World Health Organization (1996) Recommended iodine levels in salt and guidelines for monitoring their adequacy and effectiveness. (WHO/NUT/96.13). Available at URL http://whqlibdoc.who.int/hq/1996/WHO_NUT_96.13.pdf.
[33] Haldimann, M., Alt, A., Blanc, A., Blondeau, K. (2005) Iodine content of food groups. Journal of Food Composition and Analysis 18: 461-471.
[34] Schone, F., Rajendram, R. (2009): Chapter 16: Iodine in farm animals. In Comprehensive Handbook of Iodine: Nutritional, Biochemical, Pathological and Therapeutic Aspects. Eds. Preedy, V.R., Burrow, G.N., Watson, R.R., Elsevier, USA, pp. 161-170.
[35] Zimmerman, T.P., Stumbo, P., Chenard, C., Braithwaite, E., Selley, B. (2008) 2008 International Nutrient Databank Directory. Available at URL http://www.nutrientdataconf.org/DatabankDir/
International%20Nutrient%20Databank%20Directory%202008.pdf.
[36] UK Food Standards Agency (2008) UK salt intake levels heading in the right direction. Available at URL http://www.food.gov.uk/news/pressreleases/2008/jul/sodiumrep08.
[37] 翟鳳英、楊曉光主編。 (2002) 《中國居民營養與健康狀況調查報告(之二): 2002膳食與營養素攝入狀況(精裝)》。出版社:人民衛生出版社。[in Chinese only].
[38] Food and Agriculture Organization (2007) Nutritional Status Assessment and Analysis - Lesson 3: Nutritional Status Indicators (Learner Notes). Available at URL http://www.foodsec.org/DL/course/shortcourseFN/en/word/trainerresources/learnernotes0282.doc
[39] Biro, G., Hulshof, K.F.A.M., Ovesen, L., Cruz, J.A.A., for the EFCOSUM Group (2002) Selection of methodology to assess food intake, European Journal of Clinical Nutrition, 56(Suppl 2): S25-S32.